UHAS Dean urges strategic role for laboratory managers in 24-hour health system reform

The Dean of the School of Allied Health Sciences at the University of Health and Allied Sciences (UHAS), Professor Samuel Essien-Baidoo, has called for urgent policy reforms to position medical laboratory managers at the centre of Ghana’s healthcare transformation.
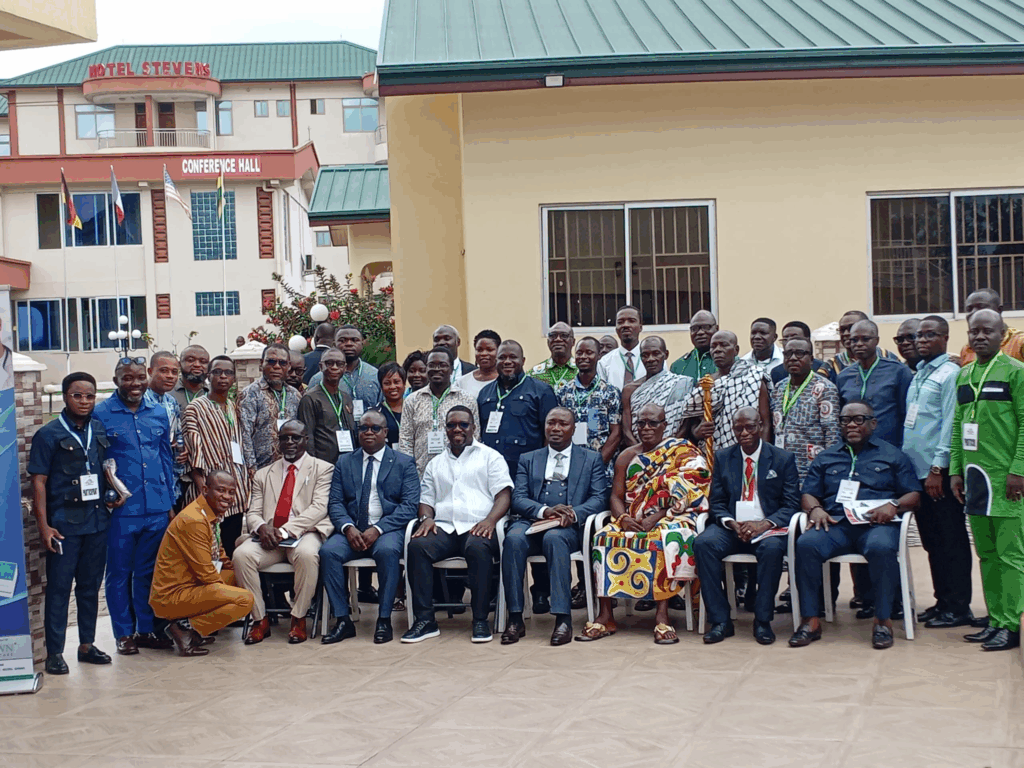
Delivering a keynote address at the Annual General Meeting of the Society of Medical Laboratory Managers, Prof. Essien-Baidoo emphasised that the full integration of laboratory managers into the healthcare governance structure is essential to achieving quality service delivery, particularly within the proposed 24-hour health economy.
“We risk crashing our healthcare system if we do not take steps now to correct this. Whether it is supporting the 24-hour health economy, leading primary healthcare diagnostics, or driving evidence-based policy, the relevance of the medical laboratory manager is unquestionable,” he stated.
The professor noted that although medical laboratory professionals played critical roles during the COVID-19 pandemic—often risking their lives and leading coordination efforts to sustain health system operations—they remain sidelined in strategic decision-making spaces.
“We are not merely technical heads. We are integral contributors to the ethical, legal, and managerial dimensions of healthcare delivery,” Prof Essien-Baidoo asserted.
He decried the fact that, out of all the teaching hospitals in the country, only two currently have Directors of Allied Health Services. He criticised attempts to suppress qualified laboratory scientists from applying for top positions, referring to recent incidents at Korle Bu Teaching Hospital as an example of institutional resistance.
“It is deeply disappointing, especially when deliberate efforts are made to circumvent the process by introducing clauses that suppress medical laboratory scientists from leadership roles,” he said.
Prof Essien-Baidoo stressed that building a resilient 24-hour health system requires leadership that goes beyond administrative competence to embrace visionary, ethical, and policy-driven engagement. He called on policymakers to redefine the role of laboratory managers, not as afterthoughts, but as cornerstones in the healthcare delivery chain.
He also urged professional bodies to intensify advocacy within the Ministry of Health, Ghana Health Service, and the private sector to institutionalise reforms that mandate the inclusion of laboratory managers in hospital directorates and governance.
“Our professional bodies must have the courage to shape institutional culture and push for reforms that empower laboratory professionals as part of the core decision-making structure,” he added.
Commending the organisers of the Annual General Meeting, Prof. Essien-Baidoo declared the meeting officially open and challenged participants to engage with the issues not as spectators but as active stakeholders.
“Let us rise to the occasion. Let us remain grounded in the laws that empower us, guided by the ethics of our profession, and inspired in our work so we can contribute wholeheartedly to national development,” he concluded.